|
Pyometra is an acute or chronic, suppurative inflammation of the uterine wall in an ovary-intact bitch. It is characterized by endometrial hyperplasia with cystic dilation of endometrial glands, along with accumulation of a neutrophil-rich exudate in the uterine lumen.Nearly 25% of bitches develop pyometra before they are 10 years of age.1 The disease is most often observed in diestrual bitches about four weeks to three months after their last ovulation. So called “stump pyometras” can occur if uterine tissue cranial to the cervix was left behind during ovariohysterectomy.
Etiology
Pyometra is an inflammatory process. The bacteria most commonly isolated from the uterus of affected individuals are uropathogenic Escherichia coli. Other bacteria, mostly vaginal commensals, such as Staphylococcus aureus, Klebsiella, Proteus and Streptococcus spp., have sometimes been recovered.8 One study reported the recovery of the same E. coli strains, as determined by biochemical fingerprinting, from the feces and the uterus of bitches with pyometra.9 The uterus is presumed to become infected via ascent of fecally-derived bacteria from the vagina during estrus, when the cervix is relaxed.
Pathogenic E. coli strains carry different uropathogenic virulence factors (UVF) that facilitate infection of the urogenital tract. Adhesive proteins at the tip of bacterial pili (fimbriae) bind to receptors on epithelial cells of the urogenital tract. Three different types of adhesins (i.e. FimH, PapGIII, Sfa) have been identified in E. coli strains isolated from bitches with pyometra.10 It has been demonstrated that FimH, the mannose-binding lectin of type-1 pili, can facilitate bacterial binding to uterine epithelial cells in some E. coli strains.11 However, other strains retained their binding ability if all three known adhesins (FimH, PapGIII, Sfa) were disabled.12 This finding suggests that factors, other than bacterial factors, are also involved. The presence of other factors is further strengthened by the observations made in a disease model that intrauterine inoculation of E. coli during estrus or anestrus did not result in pyometra but inoculation of the same strain in diestrus did.13
Pathophysiology
Pathogenesis of pyometra is incompletely understood and currently believed to be multifactorial in origin. Cystic endometrial hyperplasia (CEH) and pyometra have historically been regarded as integral components of the same disease entity. It was believed that CEH arose first and predisposed the uterus to a secondary bacterial infection. Although both diseases bear many similarities and can occur concurrently, there is evidence that both can also occur independently.2 Studies have shown that any mucosal irritant in a progesterone-influenced uterus can lead to CEH.3 Therefore, the presence of CEH in a uterus affected with pyometra could be the result of a reaction to the bacterial infection.
Factors that may influence the disease include cyclic changes in ovarian hormones, parity, breed and age of the bitch, and administration of exogenous hormones, such as estrogens for misalliance (mismating).20 The relatively long progesterone-dominated diestrous phase that is unique to the bitch seems to predispose them to pyometra. This risk is attributed to the effects progesterone has on the uterus, such as uterine stromal and glandular proliferation, leukocyte inhibition, decreased myometrial contractions, and keeping the cervix closed. These effects are exacerbated by estrogen during proestrus/estrus preceding the diestrus phase.4 The risk of uterine infection increases with each estrous cycle as these hormonal changes on the canine uterus are cumulative.5
Although there is no evidence of abnormalities of ovarian hormone concentrations being involved in the pathogenesis of pyometra, it has been shown that progesterone is necessary to initiate a CEH reaction and estrogen potentiates progesterone’s effects by up regulating the expression of progesterone receptors.4,7 The use of exogenous steroid hormones (i.e. progestagens such as megestrol acetate) for contraceptive purposes has been shown to induce the disease in dogs.
The role of the bitch’s immune response has recently been emphasized by the discovery of endometritis in the bitch.14 It was widely believed that endometritis did not exist in the canine species and a bacterial infection would always result in pyometra. Recent studies; however, showed that bacteria can be isolated from subfertile bitches that do not show the hallmark signs of pyometra. Interestingly, the mean age of these bitches was lower than in those with pyometra. These findings suggest that the uterus might contain bacteria in the form of subclinical endometritis for some time before unknown factors allow bacterial proliferation and subsequent pyometra.
E. coli infection induces a transient glomerular and tubular dysfunction in the kidneys, which leads to clinical signs of polyuria/polydipsia and the finding of low/isosthenuric specific gravity.17 Circulating cytokines may also play a role in the development of systemic disease in affected bitches.21
Diagnosis
History/Physical Examination Findings: Classically the affected bitch has a history of having been in heat within the last 12 weeks. Previous pregnancies, time elapsed since the last estrus, and administration
of any exogenous hormones should be noted. Presenting complaints include
(but are not limited to) polyuria, polydipsia, lethargy, anorexia, vomiting, and/or vaginal discharge. Pyometra must be ruled out in any ill, ovary-intact bitch. Common clinical findings include pale mucous membranes, fever, lethargy, depression, dehydration, cardiac arrhythmias, and uterine enlargement. Care should be taken during abdominal palpation as forceful palpation can result in uterine rupture.
The presence of vaginal discharge is dependent on the patency of the cervix. In an open-cervix pyometra a blood stained, purulent vaginal discharge may be the only clinical sign. Animals with closed-cervix pyometra may have no vaginal discharge and are more commonly systemically ill because resorption of bacterial toxins from the uterine lumen into the circulation can result in endotoxemia. Bacteremia may also occur.
Complete Blood Count (CBC): The leukogram frequently shows a marked neutrophilia (>35,000 x 106/L) with a left shift (± toxic change) but results can be variable. In some cases the CBC may be normal, especially if the pyometra is detected early by ultrasonography. Animals with sepsis may have leukopenia. A normocytic, normochromic, nonregenerative anemia may also be seen.
Biochemistry Panel: Hypergammaglobulinemia, hypoalbuminemia, hypercholesterolemia, elevated serum levels of C-reactive protein, acute phase protein, blood urea nitrogen (BUN), creatinine, and liver enzymes (i.e. alanine aminotransferase, alkaline phosphatase) can be present.8,24 Conflicting reports exist on blood or plasma lactate levels in affected dogs, so the assay is not considered very helpful at this time.18,19
Hormonal Assay: Progesterone concentration is >2 ng/mL with a closed-cervix pyometra.
Urinalysis: Isosthenuria, bacteriuria, glucosuria and/ or proteinuria may be found. Urine is collected by ultrasound-guided cystocentesis in order to avoid the risk of uterine puncture. A mid-stream urine sample is not recommended as it is likely to be contaminated by vaginal discharge.
Abdominal Radiography: An enlarged, distended uterus is commonly observed and can displace the
small intestines. These changes are very similar to those in early pregnancy
prior to fetal skeletal ossification (which starts 42 days after the luteinizing
hormone peak). The limitation of radiography is that it is often difficult
to differentiate pyometra from other causes of uterine enlargement, such
as mucometra, hydrometra, hemometra, and leiomyoma.
Abdominal Ultrasonography: Ultrasonography is the most important diagnostic tool in a pyometra case.
The uterine horns typically appear distended with hypo- to hyperechoic
fluid, with or without flocculation . The uterine wall is often thickened,
with irregular edges and small hypoechoic areas consistent with cystic
changes of the endometrial glands. However, the uterine wall can appear
thinner than normal if the uterus is severely distended.
Cytology & Bacterial Culture: Cytology of the uterine or vaginal discharge reveals large numbers of degenerative neutrophils and phagocytized bacteria. Ideally fluid for culture and sensitivity is collected transcervically directly from the uterus. However, if this is not possible a cranial vaginal sample can be obtained via speculum with use of a guarded swab.
Age at presentation for pyometra in dogs is typically >7 years. However, the range has been reported to be from 4 months to 16 years in dogs.6 Animals are presented most commonly within 12 weeks of their last estrus.6 Nulliparous animals are more commonly affected than multiparous ones. A breed predisposition has been proposed in dogs. In one study it was found that the three most affected breeds, the Bernese Mountain dog, Rottweiler and rough-coated collie, had a two times higher incidence of the disease than the rest of the population.1 A study of potential risk factors of canine pyometra showed that a previous pregnancy was protective for the Rottweiler, collie and Labrador retriever, but not for the golden retriever.23
SPECIFIC THERAPY
Surgical Therapy
Ovariohysterectomy, with resection of the entire cervix, is the treatment
of choice in all animals not intended for breeding. Owners of breeding
animals should be warned of the possibility of recurrence after medical
therapy. Patients may be in poor condition, so metabolic acidosis, arrhythmias,
and dehydration must be corrected before the animal undergoes anesthesia.
Intravenous fluids and antibiotics are given preoperatively (see Medical
Therapy below).
Great care should be taken in handling the uterus as it is often very friable. The cervix is removed in its entirety in order to avoid leakage of pus into the abdomen.
Medical Therapy
Medical treatment is a valid choice in young breeding animals that are systemically well, but is discouraged in bitches not intended for breeding. After stabilization of the patient, the rationale behind medical treatment for pyometra is three-fold:
- Removal of progesterone influence to allow cervical opening, uterine contraction, and improvement of local immune status
- Drainage of pus and elimination of bacteria through an open cervix aided by uterine contractions
- Prevention of further bacterial proliferation
1) Prostaglandin F2α (PGF2α) is not registered for use in companion animals but can be used off-label. It has luteolytic and ecbolic effects. It is important to start with low doses of PGF2α in order to minimize side effects, as well as the ecbolic effect of the drug, which could potentially cause uterine rupture in a closed-cervix pyometra. Once luteolysis has occurred and the cervix is open, the dose can gradually be increased, depening on the patient's tolerance to the drug, until evacuation of the uterus is achieved (desired effect of treatment).
Side effects: Side effects are dose-dependent and rarely seen with the new low-dose protocol. Improved tolerance of PGF2a and reduction of side effects occurs after each subsequent injection. Adverse signs include tachypnea, vomiting, diarrhea, urination, and anxiety. Signs usually start about 20 minutes after treatment. Walking the dog for 15 minutes after administration seems to alleviate the side effects. The animal should be hospitalized for at least one hour after treatment to observe for side effects.
Recommended dosages using naturally occurring PGF2α (e.g. dinoprost tromethamine) are 10 μg/kg SC q 8 hrs for 1 day, then 25 μg/kg SC q 8 hrs for 1 day, then 50 μg/kg SC q 8 hrs for 3-4 days or until vaginal discharge is no longer observed.15
PGF2α can be used on its own or in combination with dopamine agonists (e.g. cabergoline) or progesterone receptor antagonists (e.g. aglepristone).
2) Dopamine agonists (used off-label), which act as prolactin antagonists, can be used as early as 25 days after the luteinizing hormone (LH) peak. If used in combination with PGF2α, they potentiate the luteolytic effect, which leads to cervical opening within 24 to 48 hours.
a) Cabergoline 5 μg/kg PO once daily
b) Bromocriptine 10-20 μg/kg PO q 8 hrs given with food because it may cause vomiting, which is inadvisable in an unwell bitch
Dopamine agonists are used in combination with PGF2α. Treatment continues until all clinical signs have resolved and serum progesterone concentration is baseline.
3) Progesterone receptor antagonists, such as aglepristone (not registered in the USA), competitively bind to the progesterone receptor with greater affinity than natural progesterone. Aglepristone has minimal side effects and is a good choice to treat closed-cervix pyometra as it results in cervical opening with minimal uterine contractions. For best results, PGF2α treatment is initiated 24-48 hours after the initial dose of aglepristone. This sequence allows the cervix to open before PGF2α leads to uterine contractions, thereby aiding uterine evacuation.16 The recommended dose of aglepristone is 10 mg/kg PO on days, 1, 2, and
8. Bitches that have poor liver and/or kidney function should not be treated
with aglepristone.
Alternative Treatment Protocol Option
Catheterization of the cervix with the use of a rigid urethroscope has been described in the treatment of open- and closed cervix pyometra in dogs.15 A transcervical endoscope, as is commonly used for insemination facilitates instillation of warm saline solution containing PGF2α into the uterus. This procedure is repeated two days later if intrauterine fluid is still detected by ultrasonography. Resolution of pyometra within 3-5 days has been reported.15 Drainage of the uterus by passing a rigid pipette through the cervix, followed by lavage with 5% povidone-iodine solution and a dose of PGF2α has also been described in 8 dogs.25 Uterine rupture or leakage of pus into the abdomen after flushing has not been reported but care in patient selection for this procedure is advised.
SUPPORTIVE THERAPY
Antimicrobial therapy with a wide-spectrum antibiotic is initiated immediately. While culture and sensitivity tests are pending therapy is started immediately on the assumption that an E. coli infection is present. Excellent results have been achieved with amoxicillin/clavulanic acid (12.5-25 mg/kg PO q 8-12 hrs), enrofloxacin 10 mg/kg PO once daily, cephalosporins (e.g. cefazolin at 22 mg/kg IM, IV q 8 hrs), and potentiated sulfonamides.
Care should be taken in using these latter antibiotics in a dehydrated,
potentially septicemic animal with impaired renal and liver function. If
oral antibiotics are given, care must be taken to administer the drugs
at a different time as the prostaglandin because the latter often causes
vomiting. Antimicrobial therapy is continued for at least 14 days after resolution
of vulvar discharge and removal of all fluid from the uterine lumen as
determined by ultrasonography.
MONITORING
Postoperative monitoring for signs of shock, dehydration, sepsis, electrolyte/acid-base imbalances, hypoproteinemia, hypoglycemia and anemia is required for at least 24-48 hours following surgery. One study demonstrated that assessment of C-reactive protein, serum amyloid A component, and haptoglobin were useful in detecting postoperative complications but they are not commonly measured in clinical settings.26
Clinical improvement should be noted within 24 hours of commencing medical treatment and resolution of the disease should occur within 7 days. Dogs that do not respond well to medical treatment within 5 days have a very poor prognosis for retaining their breeding potential and ovariohysterectomy should be performed.15
Recommendations for monitoring treatment success are as follows:
- Vaginal discharge should greatly increase in volume within 24 hours of medical treatment and usually ceases in about 7-10 days.
- Vaginal cytology should show a decrease in the number of degenerative neutrophils after 5 days.
- Weekly CBCs are performed to check for decreasing neutrophilia. Usually neutrophil count is normal 10-15 days after commencement of medical therapy.
- Ultrasonography typically demonstrates visible reduction in uterine lumen size after 5 to 7 days. Treatment with prostaglandin continues until there is no fluid visible in the uterus with ultrasonography.
- Serum progesterone levels commonly decline within 48 hours of PGF2α treatment.
Optimal breeding management in the subsequent estrous cycle after pyometra treatment is recommended. High-quality semen of proven fertility should be used, in combination with timed insemination and semen extenders containing antibiotics. Frozen-thawed semen should not be used in these cases. It is essential to follow these bitches closely with vaginal cytologies and ultrasound examinations in order to detect recurrence of pyometra early. An ultrasonographic pregnancy exam about 25-30 days after the LH peak is highly recommended to detect early signs of intrauterine fluid before clinical signs associated with pyometra and septicemia occur.
PROGNOSIS
Prognosis for survival is good with medical and surgical treatment, if uterine rupture has not occurred. However, the mortality rate of bitches undergoing treatment is 4%.15 The recurrence rate of pyometra is dependent on age, parity, and preexisting uterine pathology. Variable pregnancy rates of 50-75% have been reported post-therapy.15 Bitches treated for pyometra have the same probability of developing pyometra or becoming pregnant as a naïve bitch of the same breed, age, and parity.15 In case of a new infection, ovariohysterectomy is strongly recommended.
About a month after the discontinuation of treatment an ultrasound is scheduled to assess uterine health, with particular focus on CEH changes. At this stage, CEH caused by the bacterial infection should have resolved. If noticeable CEH changes are still present, prognosis for future fertility becomes guarded.
In regard to future reproductive performance it should be noted that the disease can reoccur and it is strongly recommended the bitch be breed at the next cycle, with an ultrasound exam for pregnancy 28 days after the LH surge to exclude another pyometra infection.
Treatment with PGF2α and/or aglepristone often leads to a shortened interestrus interval that can be associated with decreased fertility at the next heat. The interestrus interval can be lengthened with an androgen-receptor agonist, such as mibolerone, in order to allow sufficient time for the uterus to remodel/recover. Mibolerone treatment is started one month after the end of medical treatment for pyometra and is administered for 2-3 months.
当院では、海外や日本の大学などで使用されております
注射薬ALIZIN(アリジン)における内科学的治療にも力を入れております。
また国内で初の猫の子宮水腫におけるALIZIN使用の発表も行いました。
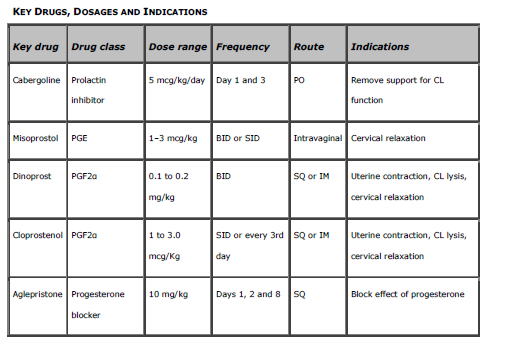
子宮蓄膿症の内科学的治療の薬剤は下記の通りですが、当院ではALIZN(アリジン)を中心に、犬・猫における選択肢の1つとして子宮蓄膿症の内科学的治療も行っております。
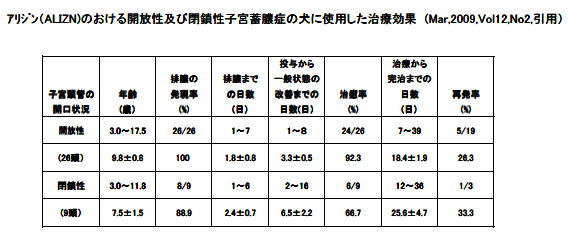
2010年米国の学会発表における子宮蓄膿症の発表の抜粋です。
|